Half of the U.S. adult population is expected to have obesity by 2030. In addition to its $172.74 billion cost burden, obesity is linked to many chronic conditions including MSK injuries. As a result, obese individuals are increasingly presenting to orthopedic practices, giving rise to the Orthobesity™ crisis. Orthopedic physicians can get ahead of this crisis with an integrated patient outreach strategy for weight loss. By supplying proactive, specific, and consistent patient engagement, orthopedic practices can transform their patients’ MSK health for the better.
Obesity & MSK Issues
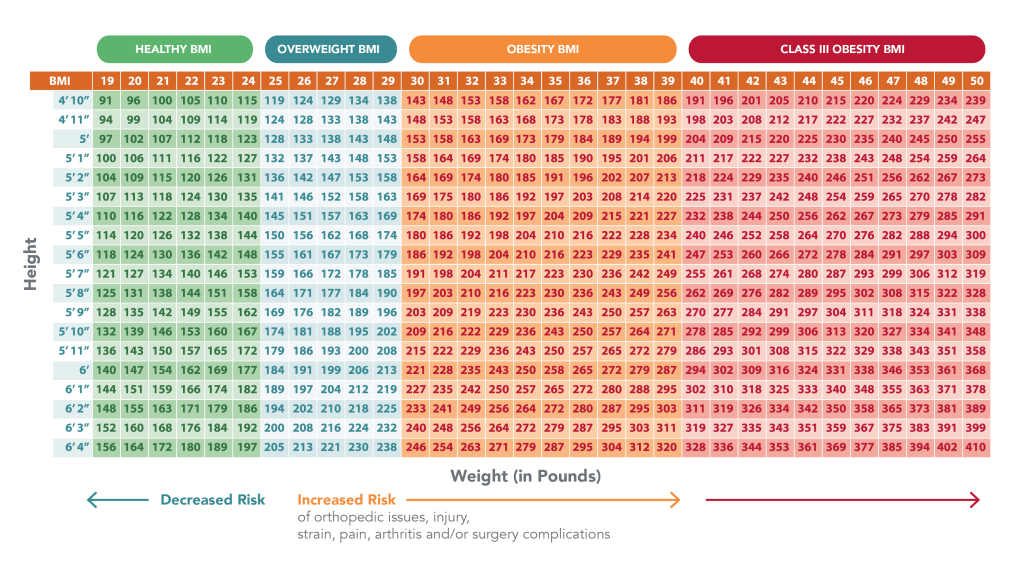
The United States has the highest rates of obesity of all the developed nations, and it’s a growing crisis. According to data from the CDC, nearly 42% of adult Americans are obese or morbidly obese with a Body Mass Index (BMI) of 30 or above. By 2030, it is estimated that nearly half of the U.S population will have obesity.
Not only does a high BMI increase the risk of type II diabetes, heart disease, and other chronic conditions, but research also points to obesity as a root cause of many musculoskeletal (MSK) conditions:
1. The odds of sustaining an MSK injury are 15% greater for overweight individuals. This figure rises to 48% for individuals with Class III obesity.1
2. Every 1 pound of excess weight causes an added 4 pounds of pressure on the knee joint and 10 pounds of pressure on the lower back.2
3. Obese individuals are 20 times more likely to require total knee replacement surgery than non-obese patients.3
4. Being overweight increases the risk of complications after surgery. For example, wound infection, pulmonary complications, deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction (MI) and others.4
Additionally, obesity significantly affects health care spending. The estimated annual medical cost of obesity in the U.S. was nearly $172.74 billion in 2019 dollars. Average annual medical costs for adults with obesity were $1,861 higher than medical costs for people with a healthy weight.5
The result is a crisis of Orthobesity™.
The Orthobesity™ Crisis: How to Help
Due to the greater likelihood of MSK complications resulting from excess weight, in addition to its growing cost burden, orthopedic physicians are facing an especially acute crisis of Orthobesity™: a trend where overweight individuals are increasingly presenting to orthopedic practices.
As a result, these practices urgently need a comprehensive approach to patient care that not only improves surgery outcomes but addresses the root causes of obesity to increase patients’ overall quality of life.
How can orthopedic physicians employ a more integrated approach to helping their patients decrease weight and improve their health? For one, the evidence is clear that messaging is a powerful factor.
A study in the Journal of General Internal Medicine found that obese patients lost significantly more weight on average when doctors supplied specific advice on how to lose weight, compared to patients who received generic advice such as “you should exercise more.”
The patients in the study who dropped more weight also joined a comprehensive weight loss program. This program gave patients access to tailored goals, educational materials, and regular check-ins with weight loss coaches.
Overall, patients in the comprehensive intervention who received specific advice from their doctors were significantly more likely to lose weight.
The science reveals that an integrated approach helps patients drop pounds. This increases the odds of a successful surgical intervention and keeps further MSK issues at bay. So, how can orthopedic physicians make the most of deploying a weight loss program for their patients?
3 Tips to Maximize the Success of your Weight Loss Program
1. Be proactive: A pair of surveys by West found that “patients want their healthcare team to be more proactive about encouraging wellness and prevention… Patients believe that if their provider pushed them to make certain changes, it would lead to better outcomes.”
How to do it: Practices can engage orthopedic patients with email or SMS outreach regarding lifestyle wellness services and advice. Including all patients can help reach not just those that need to lose weight for surgery, but patients who can benefit from preventative interventions, too.
2. Go virtual: Telemedicine is here to stay, and according to a study from the National Library of Medicine, telemedicine interventions can successfully help obese patients lose weight. These types of interventions may also improve the accessibility of treatment to hard-to-reach populations, such as the elderly.
How to do it: In addition to digital outreach, employing a virtual connected care program or remote patient monitoring service can help orthopedic practices more easily monitor their patients’ progress and provide personalized care.
3. Partner up: A weight loss program can be more effective with additional support and outreach from non-clinical staff. For example, one study found that a combination of population health management and an online program improved weight loss relative to an online-only program.6
How to do it: A comprehensive weight-loss program may seem daunting to a small practice, but you don’t have to go it alone. Prescribe FIT is a full-service remote patient monitoring solution that extends orthopedic care beyond your office with one-on-one patient coaching from certified Care Coordinators to address the root cause of their MSK issues.
Final Thoughts
Orthopedic physicians are extremely well-positioned to combat the Orthobesity™ crisis directly, and the solution is clear: proactive, specific, and consistent patient engagement. A successful patient health program may be the transformative force patients need to improve their MSK health and surgery outcomes. Orthopedic physicians need only to “Prescribe FIT.”
Published on September 1, 2022

